A Molecule From the Gut Could Transform Weight Loss Treatment
In the ongoing search for safe, effective weight management strategies, a team of researchers has identified a naturally occurring compound produced in the gut that suppresses appetite, enhances fat metabolism, and promotes healthy weight loss in preclinical studies without the gastrointestinal side effects that plague current medications. The discovery opens a promising new avenue for developing weight loss therapies that work with the body's own regulatory systems rather than overriding them pharmacologically.
The compound, a metabolite produced by specific strains of gut bacteria during the fermentation of dietary fiber, was identified through a large-scale screening of gut-derived molecules in a population cohort of over 5,000 individuals. Researchers noticed that people who maintained healthy weight over long periods had significantly higher circulating levels of this metabolite, an association that persisted after controlling for diet, exercise, age, and genetic factors.
How the Gut Molecule Works
The metabolite, which belongs to a class of compounds known as postbiotics, exerts its effects through multiple complementary mechanisms that collectively reduce energy intake and increase energy expenditure. Understanding these mechanisms required years of painstaking biochemical investigation, but the resulting picture is elegant in its coherence.
Appetite Suppression Through the Gut-Brain Axis
The compound activates receptors on enteroendocrine cells in the intestinal lining, stimulating the release of satiety hormones including peptide YY and glucagon-like peptide 1. These hormones signal to the hypothalamus, the brain region that governs appetite and energy balance, to reduce hunger and promote feelings of fullness after eating. Notably, this is the same hormonal pathway targeted by GLP-1 receptor agonist drugs such as semaglutide, but the gut metabolite activates it through the body's own signaling system rather than through an externally administered pharmaceutical agent.
In animal studies, administration of the purified compound reduced food intake by approximately 20 percent without causing the nausea, vomiting, and diarrhea commonly reported by patients taking GLP-1 drugs. The researchers attribute this tolerability to the compound's physiological mode of action: because it works through the same pathways the body uses naturally to regulate appetite, it does not overwhelm the system in the way that supraphysiological doses of synthetic GLP-1 agonists can.
Enhanced Fat Metabolism
Beyond appetite suppression, the metabolite also appears to directly enhance fat metabolism. In adipose tissue, it activates AMP-activated protein kinase, a master regulator of cellular energy balance that promotes the burning of stored fat for fuel. It also stimulates the browning of white adipose tissue, converting energy-storing fat cells into energy-burning beige adipocytes that generate heat through a process called thermogenesis.
In mouse models of diet-induced obesity, eight weeks of treatment with the compound led to a 15 percent reduction in body weight, with the majority of the lost mass coming from visceral fat, the metabolically dangerous fat that surrounds internal organs and drives insulin resistance, cardiovascular disease, and chronic inflammation.
The Microbiome Connection
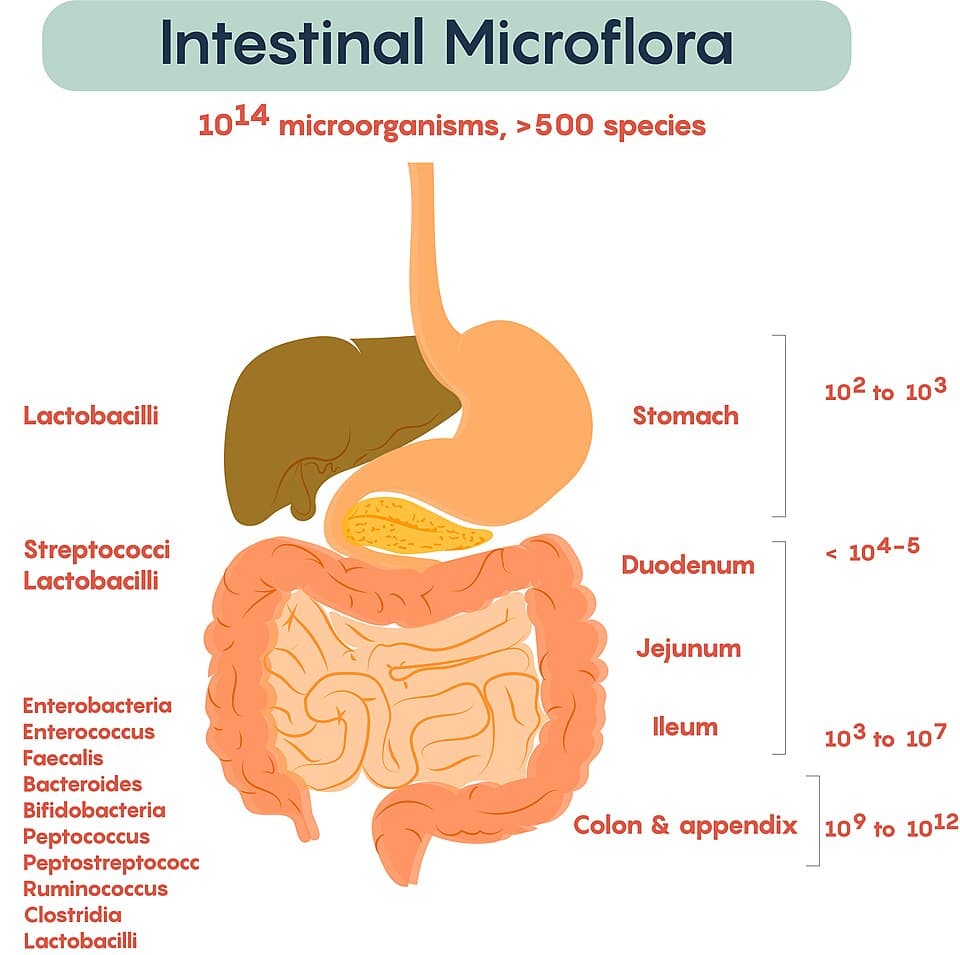
One of the most intriguing aspects of the discovery is its connection to the gut microbiome. The compound is not produced by human cells but by specific bacterial species that thrive on dietary fiber, particularly resistant starches and certain types of soluble fiber found in whole grains, legumes, fruits, and vegetables.
Why Some People Produce More Than Others
Individual variation in gut microbiome composition helps explain why some people produce higher levels of the metabolite than others. The bacterial species responsible for its production are more abundant in people who consume fiber-rich diets and are depleted in those who eat highly processed, low-fiber diets. Antibiotic use, stress, and other factors that disrupt microbial diversity also reduce the capacity to produce the compound.
This connection between diet, microbiome composition, and metabolite production provides a mechanistic explanation for the well-known but incompletely understood association between high-fiber diets and healthy weight maintenance. It also suggests that dietary interventions aimed at increasing fiber intake could boost natural production of the compound, offering a non-pharmacological approach to weight management that works through the microbiome.
Advantages Over Current Weight Loss Medications
The current landscape of weight loss pharmacotherapy is dominated by GLP-1 receptor agonists, which have demonstrated remarkable efficacy but come with significant drawbacks. Up to 40 percent of patients on semaglutide report gastrointestinal side effects including nausea, vomiting, and diarrhea. There are also concerns about muscle mass loss, gallbladder disease, and the rapid weight regain observed when patients discontinue treatment.
A Gentler Approach
The gut-derived metabolite addresses several of these limitations. Its physiological mode of action produces appetite suppression without the gastrointestinal distress associated with suprapharmacological GLP-1 stimulation. In animal studies, the compound preserved lean muscle mass during weight loss, a critical advantage given that muscle loss contributes to metabolic slowdown and reduced functional capacity.
Perhaps most significantly, the weight loss achieved with the compound appears to be more durable. Animals that received the metabolite for eight weeks and were then switched to placebo maintained a significant portion of their weight loss over a subsequent eight-week observation period, in contrast to the rapid rebound typically seen after discontinuation of GLP-1 drugs. The researchers hypothesize that the compound may help reset the body's weight set point by modifying the gut-brain signaling that governs long-term energy balance.
From Discovery to Drug Development
Translating the preclinical findings into a human therapy will require navigating several challenges. The compound's oral bioavailability, pharmacokinetics, and long-term safety profile in humans remain to be established. Phase 1 clinical trials are expected to begin later this year, with initial studies focused on safety and dose-finding in healthy volunteers before progressing to efficacy trials in people with obesity.
Multiple Delivery Strategies Under Exploration
The research team is exploring multiple delivery strategies. In addition to a purified oral formulation of the compound itself, they are investigating probiotic approaches that would deliver the producing bacteria directly to the gut, allowing patients to manufacture the metabolite endogenously. A third strategy involves dietary interventions optimized to promote growth of the relevant bacterial species, an approach that would require no pharmaceutical intervention at all.
Each strategy has its own advantages and challenges. The purified compound offers the most precise dosing but requires manufacturing at scale. The probiotic approach is conceptually appealing but faces challenges in ensuring bacterial survival through the acidic stomach environment and stable colonization of the gut. The dietary approach is the most accessible but may produce variable results depending on individual microbiome composition.
A Paradigm Shift in Weight Management
Regardless of which delivery strategy ultimately proves most practical, the discovery of a natural gut compound that safely promotes weight loss represents an important philosophical shift in obesity treatment. Rather than viewing obesity solely as a problem to be overcome with powerful pharmaceutical agents, this approach recognizes the body's own sophisticated weight-regulation systems and seeks to restore them to optimal function.
For the hundreds of millions of people worldwide struggling with overweight and obesity, and for the healthcare systems bearing the enormous cost of obesity-related disease, a safe, effective, and potentially diet-based approach to weight management would be transformative. While the road from preclinical discovery to clinical application is long, the elegance and plausibility of the science behind this gut-derived metabolite make it one of the most watched developments in metabolic medicine today.
As the lead researcher observed, the human body evolved sophisticated mechanisms for maintaining energy balance over millions of years. Modern diets and lifestyles have disrupted those mechanisms. The most promising therapeutic strategies may not be those that introduce entirely new pharmacological forces but those that help the body remember what it already knows how to do.